Contents
- 1 Overview of Diabetic retinopathy
- 2 Causes of Diabetic Retinopathy
- 3 Risk factors of Diabetic Retinopathy
- 4 Diabetic Retinopathy Prevention Tips
- 5 Kinds of Diabetic Retinopathy
- 6 Symptoms of Diabetic Retinopathy
- 7 Treatment for Diabetic retinopathy
- 8 Advanced diabetic retinopathy
- 9 Alternative medication to Diabetic retinopathy
- 10 Conclusion
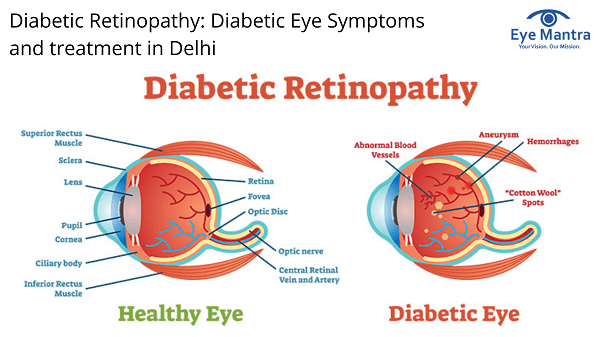
Overview of Diabetic retinopathy
Diabetic retinopathy is a diabetes condition that hits the eyes. It is caused by eye injury to the blood vessels of the light-sensitive tissue at the back of the eye (retina). In the beginning, diabetic retinopathy may generate no symptoms or only moderate vision difficulties. Ultimately, it can induce night blindness. The situation can occur in anyone who has type 1 or types 2 diabetes. The longer you have diabetes and the less controlled your blood sugar is, the more likely you are to grow this eye complication.
DR is a complexity of diabetes and a leading cause of blindness in the United States (U.S.).The retina is the membrane that covers the back of the eye. It is extremely delicate to light. It transforms any light that hits the eye into signals that can be read by the brain. This process creates visual images, and it is how to sight roles in the human eye.
Diabetic retinopathy affects the blood vessels within the retinal tissue, making them leak fluid and harm vision.
Causes of Diabetic Retinopathy
Slowly too much sugar in your blood can cause blockage of the tiny blood vessels that nourish the retina, cutting off its blood supply. As a result, the eye attempts to develop new blood vessels. But these new blood vessels don’t mature properly and can leak easily.
Anybody with diabetes is at the chance of developing diabetic retinopathy. However, there is a higher risk if the person:
- Does not correctly control blood sugar levels
- Experiences high blood pressure
- Has high cholesterol
- Is pregnant
- Smokes regularly
- Has had diabetes for a long time
A loss to the network of blood vessels that support the retina is the essential cause of diabetic retinopathy.
High glucose levels break these vessels and limit the flow of blood to the retina. The difficulties with the blood vessels can be as mild as small bulges in the vessel wall that occasionally leak blood without affecting vision.
Risk factors of Diabetic Retinopathy
Diabetes duration
The longer a person undergoes from diabetes, the higher the risk of developing retinopathy. Nearly 90% of people who have had type 1 diabetes for over 10 years develop some extent of diabetic retinopathy. The proportion of those who have had type 2 diabetics for over 10 years but do not take insulin is 67% and among type 2 diabetics with a 10-year disease span who do take insulin, the proportion is 79%.
Blood sugar level
The higher a person’s blood sugar level is, the greater the risk of developing diabetic retinopathy. People with a persistently raised glycated hemoglobin level (which indicates blood glucose level) are at greater risk of developing diabetic retinopathy.
Blood pressure
High blood pressure in itself is detrimental to the retinal blood vessels and can cause hypertensive retinopathy. Therefore, among people with both a raised blood sugar level and high blood pressure, the risk of diabetic retinopathy is greater still.
Smoking
Smokers are at a greater risk of blood vessel disorders, including retinopathy.
Gestational diabetes
Pregnant women with gestational diabetes are at a greater risk of developing diabetic retinopathy.
Diabetic Retinopathy Prevention Tips
All your diabetic retinopathy prevention efforts shall be concentrated on one key point, i.e. controlling blood sugar, blood pressure, and cholesterol levels in your body. let’s have a look at some of the effective tips for prevention from Diabetic Retinopathy.
1: Healthy Lifestyle and Healthy Diet: Your diet plays a vital role in maintaining optimal eye health, so you better adopt a healthy lifestyle focused on a healthy diet. Possible eye nutrition is the need for a healthy lifestyle.
2: Get Low on Fat Sugar and Salt: Lower down your consumption of sugar, fat, and salt.
3: Get to Your Ideal BMI: Lose weight, aiming to lie within the BMI range best suitable for you.
4: Regular Workout Regime: Follow a regular workout schedule involving at least 150 minutes of moderately intense physical activity every week. If you’re a beginner, aiming for 10,000 steps a day can be a good start for you.
5: Quit smoking: It is detrimental for your overall well being and contributes to the development of many serious eye diseases.
6: Say No to Alcohol: Similarly, you need to curb your alcohol consumption. Quitting it all together is the best way to go about it, but if you found it inevitable, make sure you don’t exceed the recommended alcohol limits. According to Dietary Guidelines for Americans, women shouldn’t consume more than a drink a day, whereas men shouldn’t exceed two drinks a day limit.
7: Monitor and Manage Your Blood Sugar Levels: This will ensure your safety against the inflictions of diabetes, diabetic eye problems. You can monitor your blood sugar levels using a couple of alternative methods, doing it by yourself as well as taking help from doctors. One way of monitoring blood sugar levels at home is through a glucose meter, which analyzes your blood sample and notifies the levels at a particular moment. Similarly, you can get your blood sugar levels reported professionally through A1C and eAG tests.
Kinds of Diabetic Retinopathy
There are 2 kinds of diabetic retinopathy:
- Early diabetic retinopathy
In this more general form — called nonproliferative diabetic retinopathy (NPDR) — new blood vessels aren’t raising (proliferating). When you have NPDR, the walls of the blood vessels in your retina strengthen downs. Tiny bulges (microaneurysms) poke out from the vessel walls of the smaller vessels, sometimes leaking fluid and blood into the retina.
Larger retinal vessels can start to expand and become irregular in diameter, as well. NPDR can progress from moderate to severe, as more blood vessels become blocked. Nerve fibers in the retina may begin to swell. Sometimes the central part of the retina (macula) begins to swell (macular edema), a condition that requires treatment.
- Advanced diabetic retinopathy
Diabetic retinopathy can grow to this more critical type, known as proliferative diabetic retinopathy. In this type, damaged blood vessels close off, creating the growth of new, abnormal blood vessels in the retina, and can leak into the clear, jelly-like material that fills the center of your eye (vitreous).
Ultimately, scar tissue stimulated by the extension of new blood vessels may create the retina to detach from the back of your eye. If the new blood vessels interfere with the normal flow of fluid out of the eye, stress may build up in the eyeball. This can harm the nerve that transfers images from your eye to your brain (optic nerve), resulting in glaucoma.
- Complications of Diabetic Retinopathy
Diabetic retinopathy includes the unusual growth of blood vessels in the retina. Complexities can commence to serious vision problems:
- Vitreous hemorrhage. The new blood vessels may bleed into the clear, jelly-like substance that fills the center of your eye. If the volume of bleeding is minute, you might see only rare dark spots (floaters). In more critical cases, blood can fill the vitreous cavity and ultimately block your vision. Vitreous hemorrhage by itself normally doesn’t cause lasting vision loss. Unless your retina is injured, your vision may revert to its previous clarity.
- Retinal detachment. The abnormal blood vessels linked with diabetic retinopathy stimulate the growth of scar tissue, which can pull the retina away from the back of the eye. This may create spots floating in your vision, flashes of light, or harsh vision loss.
- Glaucoma. New blood vessels may develop in the front part of your eye and interfere with the normal flow of fluid out of the eye, causing stress in the eye to build up (glaucoma). This pressure can harm the nerve that transfers images from your eye to your brain (optic nerve).
- Blindness. Ultimately, diabetic retinopathy, glaucoma or both can lead to entire vision loss.
Symptoms of Diabetic Retinopathy
You might not have symptoms in the initial stages of diabetic retinopathy. As the situation progresses, diabetic retinopathy indications may include:
- Spots or dark strings floating in your vision (floaters)
- Blurred vision
- Fluctuating vision
- Impaired color vision
- Dark or empty areas in your vision
- Vision loss
- Dry eyes
Diabetic retinopathy usually affects both eyes.
- If the person has fairly large, rapid shifts in their blood sugar levels, they may notice that their vision becomes blurry. This may occur before the diagnosis of diabetes mellitus, or it may develop after the initiation of treatment or a change in the treatment of diabetes mellitus. This problem with vision or focusing will disappear once blood sugar levels have been steady for approximately one week.
- Even if the person has background diabetic retinopathy or early proliferative diabetic retinopathy, it is possible that they may not have any symptoms, or they may experience mild-to-severe blurring or vision loss. Many people with critical diabetic eye disease may not understand that they have a vision problem until it is too late and permanent harm has already occurred.
- If the person has a cataract, vision may become blurry or hazy. At night, the person may experience glare from oncoming lights. They may require cataract surgery for overcoming this situation.
- If the person has glaucoma, they may not experience any symptoms until a significant loss of vision has already occurred. They may require glaucoma surgery for overcoming this situation.
- In diabetic eye disease due to diabetic retinopathy, symptoms of pain or discomfort in the eyes are normally not present.
Treatment for Diabetic retinopathy
Treatment, which depends mainly on the type of diabetic retinopathy you have and how critical it is, is geared to slowing or stopping the improvement of the condition.
Early diabetic retinopathy
If you have moderate nonproliferative diabetic retinopathy, you may not require medication right away. However, your eye doctor will strictly monitor your eyes to determine when you might require treatment.
Work with your diabetes doctor (endocrinologist) to discover if there are ways to recover your diabetes management. When diabetic retinopathy is mild or moderate, good blood sugar control can normally slow the improvement.
Advanced diabetic retinopathy
If you have proliferative diabetic retinopathy or macular edema, you’ll require immediate surgical practice. Depending on the particular difficulties with your retina, options may include:
- Photocoagulation. This laser treatment, also recognized as focal laser treatment, can prevent or slow the leakage of blood and fluid in the eye. During the procedure, leaks from abnormal blood vessels are managed with laser burns. Focal laser treatment is normally performed in your doctor’s office or eye clinic in a single session. If you had blurred vision from macular edema before surgery, the treatment might not return your vision to normal, but it’s likely to decrease the chance macular edema may worsen.
- Panretinal photocoagulation. This laser treatment, also recognized as scatter laser treatment, can shrink the unusual blood vessels. During the procedure, the areas of the retina away from the macula are managed with scattered laser burns. The burns generate unusual new blood vessels to shrink and scar. It’s normally done in your doctor’s office or eye clinic in two or more sessions. Some loss of external vision or night vision after the procedure is possible.
- Vitrectomy. This method practices a tiny surgery in your eye to extract blood from the middle of the eye (vitreous) as well as scar tissue that’s tugging on the retina. It’s performed in a surgery center or hospital using local or general anesthesia.
- Injecting medicine into the eye. Your doctor may recommend injecting medication into the vitreous in the eye. These medications, called vascular endothelial growth factor (VEGF) inhibitors, may help prevent the extension of new blood vessels by preventing the effects of growth signals the body sends to create new blood vessels. Your doctor may prescribe these medications, also called anti-VEGF therapy, as a stand-alone therapy or in combination with pan-retinal photocoagulation. While studies of anti-VEGF therapy in the treatment of diabetic retinopathy are promising, this method is not yet considered standard. Surgery often slows or stops the progression of diabetic retinopathy, but it’s not a remedy. Because diabetes is a permanent condition, future retinal damage and vision loss are still possible.
Alternative medication to Diabetic retinopathy
Numerous alternative therapies have recommended some advantages for people with diabetic retinopathy, but more research is needed to understand whether these therapies are effective and secure.
Be assured to let your doctor know if you are using any herbs or supplements. They have the potential to interact with other prescriptions or cause complexities in surgery, such as excessive bleeding.
It’s necessary not to delay standard treatments to try unproven remedies. Early treatment is the best way to block vision loss.
Conclusion
Diabetic retinopathy (DR) however is an end-organ response to a systemic disease, representing only one of many microvascular and macrovascular diabetic complications. The newer evolving techniques and technology have improved the diagnostic accuracy of screening methods and access of diabetic patients to specialist care. Despite this progress, DR remains a significant cause of acquired visual loss in working-age adults worldwide. Patients with DR are 25 times more likely to be blind than are non-diabetic patients of similar age and gender.
For any surgeries related to eyes do visit our website Visit the best Eye Hospital Delhi Now!!!
Call +91-8851044355 and book an appointment. You also mail at eyemantra1@gmail.com. Our team of great and experienced ophthalmologists will advise the best options for safely and effectively treat your dry eyes. Remember if you have any concerns about your eyes, from Retina Surgery, Specs Removal to Cataract Surgery