In case you have been diagnosed with Cataract and have been advised surgery. Most probably, your eye doctor will perform phacoemulsification or “phaco” surgery.
Phacoemulsification involves emulsifying or liquifying the natural lens of the eye. And is the latest, state-of-the-art and very safe technology to remove the cataract.
Just behind the iris, a lens is located. It focuses light on the retina, to produce clear and sharp images. The lens can change shape, known as accommodation.
With age, however, the lens hardens and loses its ability to accommodate. The entire lens is held within a lens capsule. As the eyes age, oxidative processes occur. Proteins and dead cells accumulate in the lens capsule, which causes the lens to become cloudy, gradually. The light doesn’t get focused now and gets scattered around because of this cloudiness. And the vision gets blurred and is no longer clear and sharp.
The phacoemulsification surgery technique was first introduced by Dr. Charles D. Kelman in 1967. He was working on various ideas and designs. But got his eureka moment after sitting in a dentist’s chair getting his teeth cleaned by a high-speed ultrasonic cleaner.
It revolutionized the management of cataract and visual rehabilitation. The technique has been much improved with the up-gradation in the technology and types of equipment. Thereby, the results of surgery have also undergone a huge change since then. Now we have much smaller incisions. Quality of the foldable lenses being implanted through them has also developed a lot.
Most of the cataract surgeries performed in the world today are a form of Phacoemulsification surgery only. The reason behind this is its excellent visual outcomes, patient safety, and efficacy.
Contents
Diagnosis and Symptoms
A person may have cataract for several years before the vision gets weakened enough to warrant surgery. Your eye specialist may suggest wearing eyeglasses, at first. It helps improve vision on a temporary basis. But as the lens turns cloudier, vision declines.
As the cataract develops and gets worse, you may notice below symptoms:
- the vision gets more blurred with time,
- blur is painless,
- reduced central vision,
- constant changes in prescription for corrective eye lenses,
- the glare from lights increases,
- poor vision in sunlight,
- near vision improves to the point where reading glasses may no longer be needed.
Whereas, if a younger person or a diabetic has a cataract, it grows at a much faster rate. Therefore, the ophthalmologist will recommend phacoemulsification surgery sooner in such cases. Surgery may also be recommended more quickly if the patient is suffering from some other eye disease as well. It may be Age-Related Macular Degeneration. Or in case the cataract interferes with a complete eye examination.
When symptoms worsen so much that it becomes difficult to perform the day-to-day activities, then the surgery becomes necessary. The Eye Specialist will conduct a complete ocular exam to determine the severity of the cataract and what type of surgery you need. For the denser and worse condition cataracts, the older method of extracapsular extraction is preferred.
If both eyes have a cataract, each must be treated separately.
The exam should include measuring the visual acuity under both low and high illumination, assessment of visual fields, microscopic examination of eye structures and pupil dilation, and measurement of intraocular pressure (IOP).
Finally, overall patient health is also a factor to be considered, and how it will affect the outcome of the surgery. The surgeon may ask you to undergo a complete physical examination before surgery.
Also read: Home Remedies for Cataract Prevention
Preparation for Phacoemulsification Surgery
Although instructions for preparation may differ somewhat, the patients are usually asked not to eat or drink anything after midnight before the day of the surgery.
You would be asked to disclose all prescriptions you are taking to determine if any of them will interfere with the surgery, and can be discontinued. Those patients who take aspirin or some other medicine for blood-thinning, usually are asked to stop for two weeks before the day of the surgery. Such medications may put you at risk for intraocular bleeding or hemorrhage. Your eye doctor will be the best judge of what course of action is to be taken.
The eye surgeon may also request you to start using antibiotic drops before the surgery to limit the chance of infection.
An A-scan measurement, which ascertains the length of the eyeball, will be performed. It helps determine what refractive power should the Intra Ocular Lens must-have. Some other pre-surgical testing such as a chest x-ray, blood test, or urinalysis may be recommended if other medical problems exist with the patient.
Mostly after the Cataract surgery, the patient is discharged quite soon. So they must be accompanied by someone, who would take them home after the surgery.
On the day of the surgery, the eye surgeon will review the pre-surgical tests and insert dilating eye drops, antibiotic drops, and a corticosteroid or nonsteroidal anti-inflammatory drop.
Anesthetic eye drops will be put in both eyes to keep both eyes comfortable during the surgery. Local anesthesia will be administered only. Patients are awake during surgery.
Sterile drapes are placed over the shoulders and head of the patient. You would be required to lie still and focus on a light overhead. A speculum is inserted to hold the eyelids open.
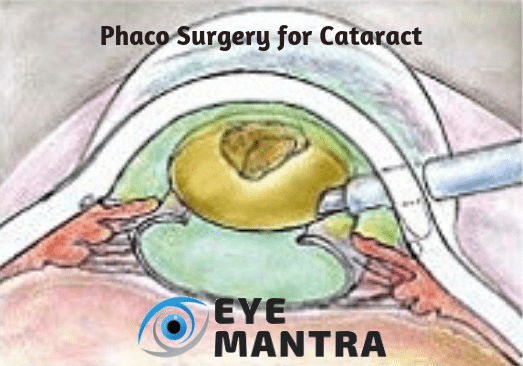
Phacoemulsification Surgery
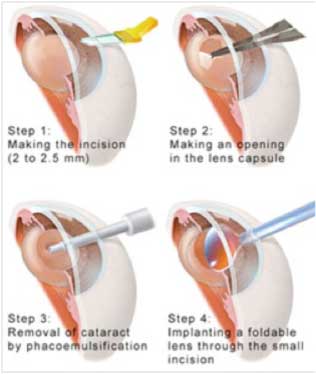
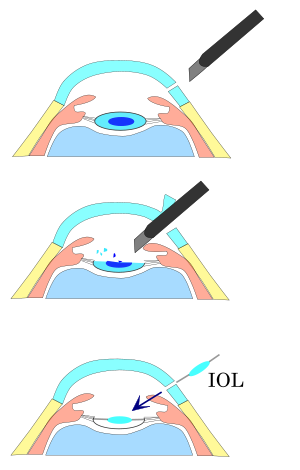
- Two tiny incisions, measuring around 2mm in length, are made in the clear cornea, the clear part of the eye, where it meets the white part of the eye, called sclera.
- A bent needle is then inserted into the front compartment of the eye, called anterior chamber and a circular opening is created on the lens surface or anterior capsule.
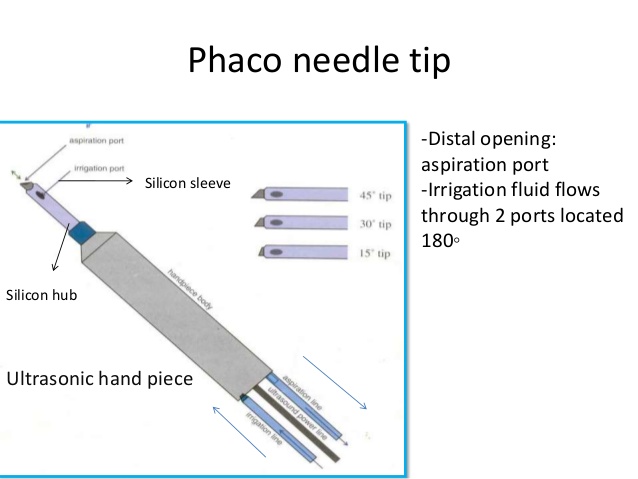
- A small instrument, phaco probe or phaco needle, is inserted into the eye. This is powered by ultrasonic energy.
- Then high-frequency ultrasound waves are used to break or emulsify the cataract into small pieces.
- The liquefied pieces of the cataract are then sucked out using the process of irrigation by vacuuming.
- In this process, the posterior capsule of the lens remains uninjured. It forms the scaffolding on which the IOL is placed.
- The IOL is implanted inside the lens capsular bag, which constitutes the posterior capsule and the remnants of the anterior capsule. This is where the circular incision was initially made.
- Recent innovations in foldable and other premium IOLs significantly shorten the time for visual recovery.
- The corneal incisions do not require stitches or sutures usually and are self-sealing because of their wound architecture.
After the Phacoemulsification Surgery
Immediately after the surgery, the patient is to wait in the outpatient recovery area to be monitored. You will be advised to rest for at least 24 hours when you will be asked to return to the Eye Hospital Delhi for a follow-up. Only light meals are advised on the day of surgery. You may still feel a bit drowsy or may even experience slight eye strain or discomfort. Usually, some over-the-counter medications may also be advised for pain relief, but you must check first with the doctor.
If you face any other side effects, for example, severe pain, nausea, or vomiting, you must report it to your surgeon immediately.
You may feel some changes in the eye during recovery. Some patients also see dark spots. But these disappear within a few weeks after surgery. There might be some discharge and itching, also. Patients may use a warm, moist cloth to put on the eyes for 15 minutes at a time for relief and to loosen any particles on eyelashes, etc. The particles should be gently cleared away with soft tissue, not a fingertip. You may even experience some pain and sensitivity to light. Some patients may also have slight bruising or drooping which will improve as the eye heals.
Patients are asked to visit the Eye Hospital Delhi on the day after the surgery. Your Eye Specialist will remove the eye cover and prescribe eye drops to prevent infections and control pressure from the IOL. These eye drops are to be used for about a month after surgery.
Next exams are usually at 1 week, 3 weeks, and 6 to 8 weeks following surgery.
Meanwhile, you will be advised to wear eye cover while sleeping for 1 to 2 weeks. And no eye rubbing. During this time, you may be asked to wear special tinted sunglasses or the current prescription eyeglasses to prevent possible eye trauma from accidental rubbing or bumping. Unlike other types of cataract extraction, patients can resume normal activity almost immediately after phaco.
After the eyes are healed completely, you will probably need new corrective lenses, at least for close vision.
Important Factors Concerning Phacoemulsification Surgery
Ophthalmologist
Choosing the right eye surgeon is crucial to the success of the operation because her expertise in this surgical technique is the main deciding factor of the outcomes of cataract surgery. Phacoemulsification surgery is a highly sophisticated method that depends on the surgical skill and experience of the performing doctor. It is essential that you choose a doctor with whom you can comfortably discuss your medical conditions. A good ophthalmologist will explain the risks and benefits of the surgery in detail, and assist you in making an informed decision about your eye health and visual needs.
Hospital
Selecting the right facility is important because it determines the operation theatre. Best Eye Hospital Delhi should be free from any possible contamination to ensure protection from infections. The right patient experience in pleasant surroundings will bring a feeling of well-being.
Technique and lenses
The Eye Specialist will determine which surgical procedure will bring the desired results only after a thorough Eye Testing is done. Transplanting Premium IOLs provide better optics, therefore, they usually get better visual results. They minimize optical irregularities and neutralize some refractive errors, including astigmatism.
Eye status
The last, but not the least determinant of surgical success is your eye health. If the patient is not suffering from any other eye diseases like corneal opacity and diseases, retinal disorders like age-related macular degeneration, glaucoma, In that case, the outcome of the surgery is excellent. Pre-existing refractive errors can usually be compensated for by choosing the appropriate IOL for the implant.
Risks
Complications occur in the rarest of rare cases. When a patient experiences spontaneous bleeding from the wound and recurrent inflammation after surgery. Flashing, floaters, and double vision are still there, even a few weeks after surgery. Such symptoms must be promptly brought to the notice of the surgeon. Some problems can easily be treated, while floaters, etc. may be a sign of a retinal detachment.
Retinal detachment is a very serious likely complication. The retina becomes detached by the surgery if there is any weakness in the retina. This complication may not be felt even after a few weeks or months.
Infections are another possible complication. The most serious one is Endophthalmitis. it is an infection in the eyeball. This problem, once widely reported, has become quite uncommon today because of better surgery techniques and antibiotics.
Patients may also be concerned that their IOL might become displaced, but innovations in the field of IOLs also have limited reports of intraocular lens dislocation.
Other potential complications are the onset of glaucoma.
It is also likely that a secondary cataract may develop in the remaining part of the capsule. This can happen for as long as one to two years after surgery. YAG capsulotomy is most often used for the secondary cataract. This outpatient procedure uses a laser and requires no incision. The laser creates a small opening in the remaining back part of the lens to allow light to penetrate.
Conventional or Phacoemulsification Surgery: a Comparison
In the Extracapsular cataract surgery, the conventional method, the incision measures around 11mm and needs multiple stitches for closure. It may also require a suture removal at a later date.
The circular opening of the lens capsule in phacoemulsification surgery as compared to the irregular opening in conventional cataract surgery results in better stability of the IOL.
The incidence of surgically induced corneal astigmatism is less with phaco surgery. So the patient may not need glasses after the surgery.
The quicker and less complex phacoemulsification surgery means that the patient spends less time in the hospital during and after surgery. It reduces the economic burden on the patients and family. As the visual functions recover faster in cataract patients, they can return to work earlier, as well.
Potentially threatening sight-threatening complications like vitreous loss, cystoid macular edema, wound leak, retinal detachment and endophthalmitis occur much less. Due to the increased safety and efficacy of the phacoemulsification surgery procedure than conventional ones.
Advantages
- The vision is better than ever before, mostly, because the implanted IOL compensates for the earlier refractive error.
- Patients can choose to have special lenses that correct for distance alone (monofocal lenses), near and distance both (multifocal lenses) and even astigmatism (toric lenses).
- Much smaller incisions that do not require stitches or sutures.
- Better vision results in better mobility, better confidence.
- Another psychological result is the immense relief from the fear of blindness.
- Most patients report a clearer vision.
- Recovery time is much less, so the patients can resume their usual activities within two to three days of surgery. Whether it is watching TV, reading or official duties also.
Disadvantages
The disadvantages of the technique are few. Moreover, they are mostly due to the cost and availability of the machine and instrumentation. In poorly developed countries, this is the biggest hurdle to its adoption.
- Devices and instruments are expensive. It acts as a deterrent in many not so well-to-do parts of the world.
- The use of disposable equipment adds to the cost of surgery.
- Not all medical schools provide surgical skill and training, or even hands-on experience.
- Because of the lack of extensive training, the technicians do not gain much experience, in comparison to conventional cataract surgery. This lack of experience results in surgical complications like corneal damage.
- Some patients get anxious and may fidget during the operation. Phacoemulsification surgery requires a cooperative patient.
If you are looking for the phacoemulsification technique or some other less expensive cataract surgery options, visit EyeMantra today.
Call NOW at +91-8851044355.
Or you can mail at eyemantra1@gmail.com
Our other services include Retina Surgery, Specs Removal, Low Vision Aids, which can help in correcting your vision.
You may also like:
Diet & Nutrition for healthy eyes