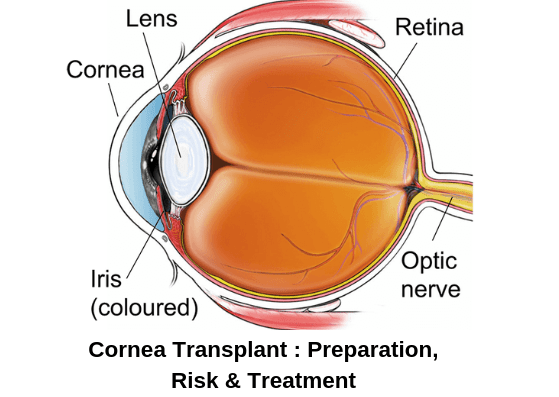
A cornea transplant (keratoplasty) is a surgical procedure to replace a portion of your cornea with corneal tissue from a donor. The cornea is the transparent, dome-shaped surface of your eye that accounts for a considerable part of your eye’s focusing power. A cornea transplant can restore vision, decrease pain and enhance the appearance of a damaged or diseased cornea. Almost all corneal transplant procedures are successful. But cornea transplant carries a little risk of complications, such as rejection of the donor cornea.
Contents
Why Cornea Transplant?
A cornea transplant is commonly used to restore blurred vision to a person who has a damaged cornea. A cornea transplant may also reduce pain or other signs and symptoms connected with diseases of the cornea.
Several conditions can be treated with a cornea transplant, including:
- A cornea that bulges outward (keratoconus)
- Fuchs’ dystrophy
- Thinning of the cornea
- Cornea scarring, caused by infection or eye injury
- Clouding of the cornea
- Swelling of the cornea
- Corneal ulcers, including those caused by infection
- Complications caused by previous eye surgery
Risks of Cornea Transplant
A cornea transplant is a comparatively safe procedure. Still, it does bring a small risk of serious complications, such as:
- Eye infection
- Enhanced risk of clouding of the eye’s lens (cataract)
- Pressure expansion within the eyeball (glaucoma)
- Difficulties with the stitches used to secure the donor cornea
- Rejection of the donor cornea
- Abrasion of the cornea
Signs and symptoms of cornea rejection
In some instances, your body’s immune system may falsely attack the donor cornea. This is called rejection, and it may need medical treatment or another cornea transplant.
Make an appointment with your eye doctor if you see any signs and symptoms of rejection, such as:
- Lack of vision
- Pain
- Redness
- Sensitivity to light
Rejection happens in about 10 percent of cornea transplants.
How to prepare for Cornea Transplant
Before cornea transplant surgery, you will experience:
- A precise eye exam: Your eye doctor examines conditions that may cause difficulties after surgery.
- Measurements of your eye: Your eye doctor ascertains what size donor cornea you require.
- An outline of all medications and supplements you’re taking: You may need to stop taking some medications or supplements before or after your cornea transplant.
- Treatment for other eye problems: Independent eye problems, such as infection or inflammation, may decrease your chances of a successful cornea transplant. Your eye doctor will operate to treat those problems before your surgery.
Your doctor will discuss what to anticipate during the procedure and describe the risks of the procedure.
Finding a donor cornea
Most corneas used in cornea transplants come from dead donors. Unlike with organs such as livers and kidneys, people needing cornea transplants generally will not need to endure long waits. That’s because many people specifically request that their corneas be available for donation after they die unless they have had certain conditions, so more corneas are available for transplantation.
Corneas may not be used from donors who had several conditions, such as certain central nervous system conditions, infections, and prior eye surgery or eye conditions, or from people who died from an unknown cause.
What will happen
During the procedure
On the day of your cornea transplant, you’ll be given a medicine to help you relax and a local anesthetic to numb your eye. You won’t be asleep during the surgery, but you wouldn’t feel any pain.
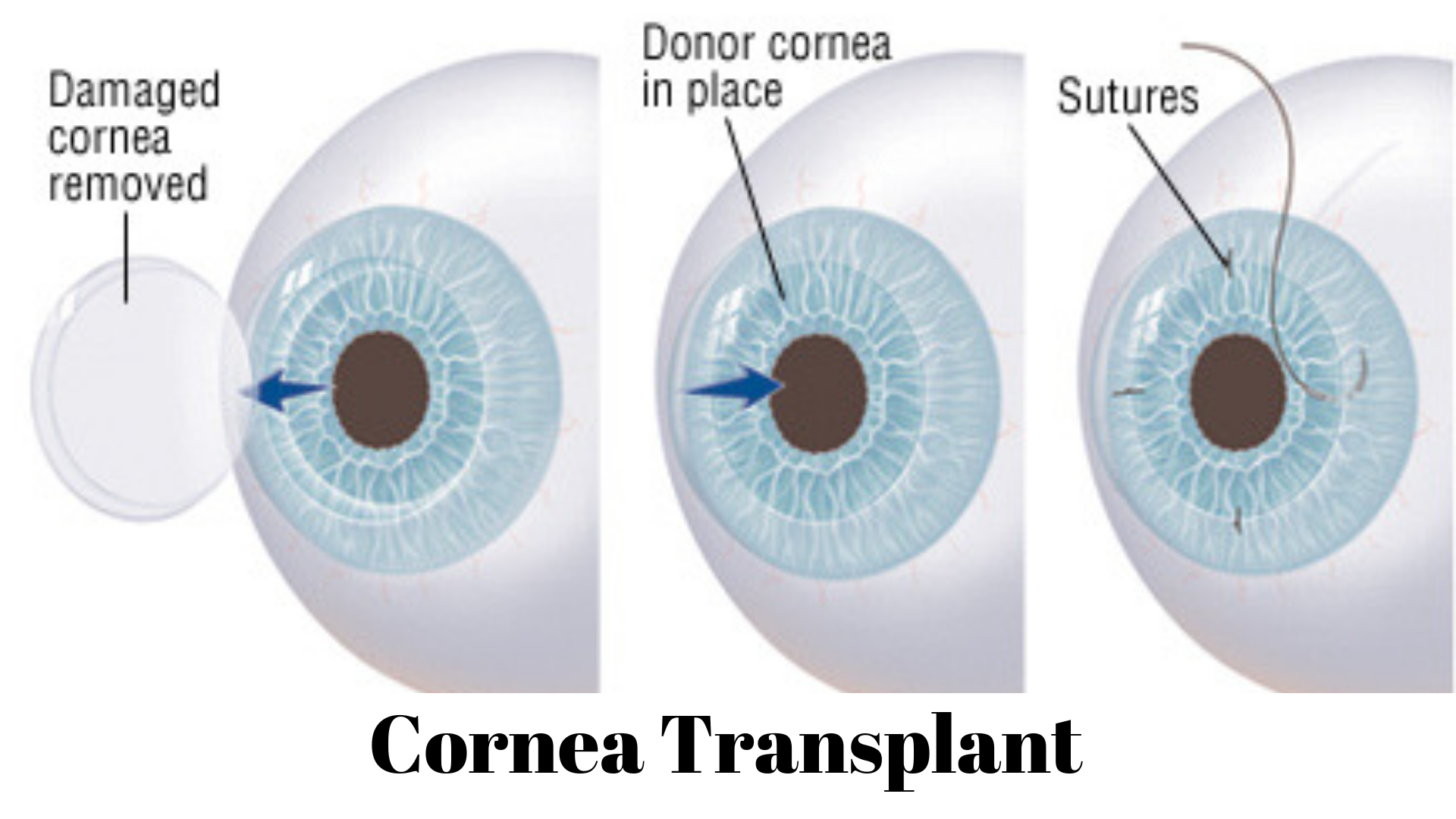
During the most common type of cornea transplant (penetrating keratoplasty), your surgeon cuts through the whole thickness of the abnormal or diseased cornea to remove a small button-sized disk of corneal tissue. An instrument that functions like a cookie cutter (trephine) is used to make this exact circular cut.
The donor cornea, cut to fit, is installed in the opening. Your surgeon then handles a fine thread to stitch the new cornea into place. The stitches may be discharged at a later visit when you see your eye doctor.
In some cases, if people aren’t suitable for a cornea transplant from a donor cornea, doctors may implant an artificial cornea (keratoprosthesis).
Procedures to transplant a portion of the cornea
With some types of cornea difficulties, a full-thickness cornea transplant isn’t always the most suitable treatment. Other types of transplants may be used that remove only certain layers of corneal tissue, or only tissue affected by the disease. These types of procedures include:
- Endothelial keratoplasty (EK): This procedure separates diseased tissue from the back corneal layers, including the endothelium, along with the Descemet membrane, a thin layer of tissue that preserves the endothelium from injury and infection. Donor tissue is precisely implanted to restore the removed tissue. There are two kinds of endothelial keratoplasty. The most common type, called Descemet stripping endothelial keratoplasty (DSEK), uses donor tissue to restore about one-third of the cornea. A newer type of procedure, called Descemet membrane endothelial keratoplasty (DMEK), uses a greatly thinner layer of donor tissue. Because the tissue used in DMEK is remarkably thin and delicate, this procedure is more challenging than DSEK, and not as usually used.
- Anterior lamellar keratoplasty (ALK): This procedure eliminates diseased tissue from the front corneal layers, including the epithelium and the stroma, but gives the back endothelial layer in place. The depth of cornea damage defines the type of ALK procedure that’s appropriate for you. Superficial anterior lamellar keratoplasty (SALK) restores only the front layers of your cornea, giving the healthy endothelium intact. A deep anterior lamellar transplant (DALK) procedure is used when cornea damage reaches deeper into the stroma. In DALK, a small hole is made in the side of your eyeball to support for removal of your cornea’s front and middle layers without breaking the back layers. Healthy tissue from a donor is then attached (grafted) to replace the removed portion.
After the procedure
Once your cornea transplant is performed, you can suppose to:
- Receive several medications: Eyedrops and, sometimes, oral medications immediately after cornea transplant and during recovery will help control infection, swelling, and pain.
- Wear an eye patch: An eye patch may guard your eye as it heals after your surgery.
- Protect your eye from injury: Take it easy after your cornea transplant, and gently work your way up to your regular activities, including exercise. For the rest of your life, you’ll need to take additional precautions to avoid injuring your eye.
- Return for frequent follow-up exams: Demand frequent eye exams in which your doctor examines for complications in the first year after surgery.
Vision correction after surgery
Your vision may initially be worse than before your surgery as your eye adapts to the new cornea. It may take many months for your vision to improve.
Once the outer layer of your cornea has improved — several weeks to several months after surgery — your eye doctor will operate to make changes that can enhance your vision, such as:
- Correcting unevenness in your cornea (astigmatism): The stitches that hold the donor cornea in place on your eye may create holes and cracks in your cornea, making your vision blurry in places. Your doctor may correct some of this by clearing some stitches and tightening others.
- Correcting vision problems: Refractive errors, such as nearsightedness and farsightedness, can be corrected with glasses, contact lenses or, in some cases, laser eye surgery.
Conclusion
Most people who undergo a cornea transplant will have their vision at least partly restored. What you can expect after your cornea transplant depends on the purpose of your surgery and your health. Your risk of complications and cornea rejection remains for years after your cornea transplant. For this purpose, expect to see your eye doctor annually. Cornea rejection can usually be managed with medications.
For the treatment of cornea, visit our website Eyemantra and book an appointment. You can also call at +91-8851044355. Or mail us at eyemantra1@gmail.com.
Our other services include Glaucoma Surgery, Specs Removal, Computer Vision Syndrome, and many more.
Related Articles:
Best Tips for Eye Care in Pollution